Be Updated With the Advances of Telehealth
The following is an excerpt from an article regarding FBI guidelines for Zoom Cybersecurity.
As individuals continue the transition to online lessons and meetings, the FBI recommends exercising due diligence and caution in your cybersecurity efforts. The following steps can be taken to mitigate teleconference hijacking threats:
- Do not make meetings or classrooms public. In Zoom, there are two options to make a meeting private: require a meeting password or use the waiting room feature and control the admittance of guests.
- Do not share a link to unrestricted publicly available social media post. Provide the link directly to specific people.
- Manage screensharing options. In Zoom, change screensharing to “Host Only.”
- Ensure users are using the updated version of remote access/meeting applications. On April 1, 2020 Zoom updated their software. In previous security updates, Zoom added passwords by default for meetings and disabled the ability to randomly scan for meetings to join.
- Manage screen recording options. Change to “Host Only.”
All of these precautions are taken by Secure Telehealth. The only responsibility our customers have is to comply with number 2 above.
Secure Telehealth customers are also exempt from email harvesting because the emails being harvested are in our domain xxx@securetelehealth.com.
Your Zoom rooms and emails are safe because you chose Secure Telehealth to manage them!
Blue Valley Behavioral Health uses Secure Telehealth to expand their services.
Here is an exerpt from an article that appeared in the Lincoln Journal Star
"Four years ago, the average wait for service at Blue Valley Behavioral Health in Southeast Nebraska stretched to three months, executive director Jon Day said. His goal has been to expand service to clients across the 16 counties Blue Valley serves.
So Blue Valley turned to a telehealth network connecting its 12 offices, allowing clients in Falls City to see a counselor in Lincoln if need be, Day said. After they implemented it in 2014, telehealth served 200 Blue Valley clients. This year, Day expects telehealth to serve 1,000 people.
That’s helped cut down waits for service to about a month, and the organization has seen 20 percent growth in the number of clients served.

"What is Telehealth and Can I use it?"
A guide to implementing telehealth services in your clinic or practice.
At any time while you are reading this, if you have any questions or just want to learn more, click here to contact us or
call (412) 837-9320.
So perhaps you have heard of "telehealth" but you are not quite sure what it is and how you may be able to use it. We get questions like this all of the time, you've come to the right place. Telehealth is defined as "the provision of healthcare remotely by means of telecommunication technology" and what you may not know is that all over the United States, providers are seeing patients through video conference. While each state has different rules and procedures for how private insurance companies and medicaid pay for those visits, (click here to learn more) there are many areas that are consistent throughout all or most of the country.
- Your first step is to choose your telehealth software provider. The most effective software is the the simplest. Your best chance for success is when the product becomes so easy to use that is as simple as and as effective as a face to face appointment. Some software providers bundle the Psychiatrists in with the software. If you are in need of a provider for your clinic, this may be the way to go, but many organizations have a provider or two, they just want to use them more effectively. Other software programs bundle and EMR and the telehealth video together in one package as well. Since the majority of telehealth providers also see patients in person, ths would complicate matters by causing an organization to switch EMR programs or have patient information in more than one area.
- Telehealth programs fail too often due to technical issues. Whether you are working with patients at home or in multiple clinic locations, thigs can go wrong. When help is always one call away, and when you call and a real person familiar with your particular situation answers the phone, then you know that your problems will be fixed quickly and you can get back to what you do best, which is help people. Providers should not have to be their own tech support team and solutions should be implemented quickly so that there is no interruption of care.
- Your Telehealth program should obviously be compliant with all HIPAA laws. Telehealth sessions should be encrypted as the information travels through the internet and providers should sign a HIPAA Business Associate Agreement (BAA) with you. Software can also have the ability to lock people out of a meeting so it is not interrupted. A waiting room is a nice feature so that a patient only gets let in to the virtual meeting room when the provider lets them in. Contact us to learn more about how to keep your patient information secure and eliminate any problems with HIPAA security.
- At Secure Telehealth, we believe that seeing patients solves many problems that providers and clinics have and is in fact the "Doctor's house call" of the future. You can see more patients, eliminate the long wait times between appointments, and save money and time by not travelling or commuting as much. We take care of your telehealth program so that you can focus on what you do best, which is helping people get better.
Nebraska law enforcement officials are using Secure Telehealth in their vehicle laptops to allow mental health evaluations of at-risk individuals on the spot.
The evaluating counselors are made available through the Targeted Adult Service Coordination Program, begun in 2005 to provide crisis response assistance to law enforcement and local hospitals dealing with people struggling with behavioral health problems. The counselors respond to law enforcement calls to provide consultation, assistance in recognizing a client’s needs and help with identifying resources to meet those needs. The no-charge service is offered to 35 sheriffs, municipal and other departments in 16 rural counties in the southeast section of the Cornhusker state.
COLUMBIA - Officials say a state telepsychiatry program supported by the Duke Endowment has been used thousands of times in hospital emergency rooms since it was installed in 2009.
In an effort to meet the critical shortage of psychiatrists in South Carolina’s underserved areas, the state’s mental health agency utilizes real-time, state-of-the-art video-and-voice technology that connects qualified psychiatrists to participating hospitals throughout the state, according to the governor’s office.
These consultations have increased the quality and timeliness of assessment and initial treatment of patients, officials say, reduced the length of stay in emergency departments for many patients, and allowed participating hospitals to direct critical personnel and financial resources to other needs.
“From the very beginning, we made it clear that South Carolina had a moral responsibility to correct longstanding issues and restore the public’s confidence in the Department of Mental Health,” said Gov. Nikki Haley. “The department lacked the appropriate funding and it was clear that our citizens were needlessly suffering. With partners like Duke Endowment and cutting edge advancements like the Telepsychiatry Consultation Program, we are now delivering mental health care where it’s needed, when it’s needed, while improving overall patient care and reducing costs and that is exactly the way it should be.”
An ongoing study of the program’s impact on medical costs by the University of South Carolina School of Medicine has determined that there is an overall medical cost savings of more than $1,700 per episode of care for patients receiving treatment via telepsychiatry, according to Haley’s office. The study has also found that patients discharged following an SCDMH telepsychiatry consultation have a significantly higher rate of accessing mental health aftercare in the community, thereby reducing their risk of readmission to an emergency department.
“The program saves money, but it’s biggest benefit is that it helps patients. Not only are many patients able to leave the emergency room sooner and return to their families, but even those patients who remain hospitalized are benefiting from the treatment recommendations of an experienced psychiatrist,” said SCDMH Director John H. Magill.
Since March 29, 2009, SCDMH has completed approximately 16,800 telepsychiatry consultations with hospital emergency departments, Haley’s office said. The SCDMH Telepsychiatry Consultation Program currently provides comprehensive consultations to 18 South Carolina hospital emergency departments.
“We are proud to be part of developing this national model and bringing it to fruition,” said Minor Shaw, Chairman of the board of The Duke Endowment. “The Duke Endowment recognizes the value of new technologies that will improve lives and strengthen communities just as DMH’s telepsychiatry program does.”
Written by
Tim Smith
Columbia bureau
FILED UNDER
News
ATA Responds to CMS Proposal for Expanded Telemedicine Coverage
July 12, 2013 (Washington, DC) - The American Telemedicine Association voices its cautious support for new proposals by the Centers for Medicare and Medicaid Services (CMS) that would expand Medicare’s telehealth footprint. CMS proposes to increase the number of beneficiaries eligible for telemedicine by modifying their urban/rural definitions and proposes several new reimbursable telemedicine services.
“Overall, the proposed rules are good news for Medicare patients and forward-thinking healthcare providers. We applaud CMS for taking steps to help these patients benefit from proven telemedicine technologies,” said Jonathan Linkous, Chief Executive Officer of the American Telemedicine Association. "But many potential beneficiaries are still left behind. For example, we hope that either CMS or Congress take additional steps to restore telehealth benefits to the one million beneficiaries in 104 counties that lost coverage last year due to reclassification to metropolitan areas.”
The proposed Medicare Physician Fee Schedule for 2014 includes two major changes that positively impact telemedicine.
The first change would extend reimbursable telehealth services to “originating sites” serving nearly one million rural beneficiaries living in large metropolitan areas. Currently, Medicare uses a strict county-based classification to enforce its rural-only rule for telemedicine coverage, leaving areas such as Death Valley and the Grand Canyon outside of the former definition and ineligible for telemedicine coverage. The new rule would create a more precise urban/rural distinction based on geographically smaller census tracts. Some critics, however, have cited the proposed rules as adding a complicated formula to the process that requires local clinics and providers to search hard-to-find census tract information to determine their eligibility.
The second proposed change would increase coverage for transitional care management services under Current Procedural Terminology (CPT) codes 99495 and 99496, involving post-discharge communication with a patient and/or caregiver. Reimbursement of these services will help healthcare providers deliver improved in-home care to at-risk beneficiaries and significantly reduce needless hospital readmissions.
CMS’ proposed rulemaking is available at http://www.ofr.gov/OFRUpload/OFRData/2013-16547_PI.pdf and will be published in the Federal Register on July 19. The proposal is currently open for comment and ATA encourages all telemedicine advocates to express their support.
The American Telemedicine Association has published a summary of telehealth provisions in the Patient Protection and Affordable Care Act of 2010. You may read it here.

Click Here to download a 9-page 2013 Coding Changes FAQ document from the American Psychiatric Association (APA)
- The CPT codes for most psychiatric services will be changing on January 1, 2013. According to the American Psychiatric Association and American Psychological Association, the most obvious change is the replacement of psychotherapy codes (e.g. 90804, 90806 and 90808) with time-specific codes:
- 90832 = 30 minutes
- 90834 = 45 minutes
- 90837 = 60 minutes
And corresponding psychotherapy codes that include evaluation and management (E/M) services.
- CPT code 90801 (Psychiatric diagnostic interview examination) will be replaced with two codes: one with and one without E/M services.
- It is unknown at this point if there will be a replacement for 90808 (75-80 min.). 90837, the code for a 60-minute session, may be considered a crisis code requiring preauthorization, much as many insurers currently treat code 90808 (Individual psychotherapy…approximately 75-80 minutes face-to-face) as a crisis code. There will be new codes for crisis psychotherapy.
- CPT code 90862 (Pharmacologic management, including prescription, use, and review of medication with no more than minimal medical psychotherapy) will be eliminated and prescribers will have to use E/M coding with stricter documentation requirements.
FAMILY AND GROUP PSYCHOTHERAPY CODES ARE NOT CHANGING
Secure Telehealth welcomes Apple Mac users, who can now connect with other Mac or Windows PC's for telemedicine!
Contact us for a demo on your Mac with OS X.
Proposed Medicare Telehealth Additions for 2013
CMS has proposed to extend reimbursement for the following services provided via telehealth:
- Annual alcohol misuse screening G0442
- Brief behavioral counseling for alcohol misuse G0443
- Annual face-to-face intensive behavioral therapy for cardiovascular disease G0446
- Annual depression screening G0444
- Behavioral counseling for obesity G0447
- Semi-annual high intensity behavioral counseling to prevent sexually transmitted infections G0445
As with all Medicare reimbursement for telehealth, the telehealth expansion would be limited to beneficiaries who receive services at an approved originating site. Generally, originating sites eligible to provide the telehealth benefit are located in a rural health professional shortage area or in a county outside of a metropolitan statistical area.
Read here for the requested rule change published in the July 30, 2012 Federal Register
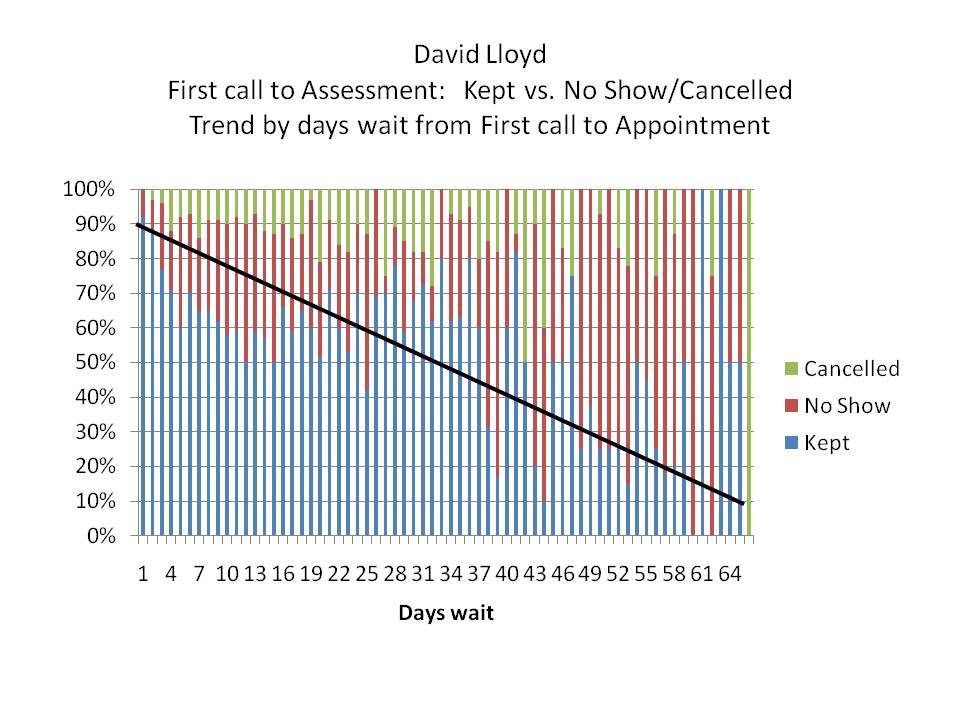
This chart created by David Lloyd shows the harm caused by delaying appointments to see the Doctor. Cancellations and No-shows increase by 10% for every seven days delay.
Secure Telehealth suggests using telehealth as a service delivery method to reduce delays.
Medicare will pay for more telehealth in 2011
The Centers for Medicare and Medicaid Services (CMS) finalized all of their proposed telehealth code additions that were originally published in June 2010. These changes will go into effect January 1, 2011.
CMS finalized their proposals to add the following requested services to the list of Medicare telehealth services for CY 2011:
Individual and group kidney disease education (KDE) services (HCPCS codes G0420 and G0421, respectively);
Individual and group diabetes self-management training (DSMT) services, with a minimum of 1 hour of in-person instruction to be furnished in the year following the initial DSMT service to ensure effective injection training (HCPCS codes G0108 and G0109, respectively);
Group medical nutrition therapy (MNT) and health and behavior assessment and intervention (HBAI) services (CPT codes 97804, and 96153 and 96154, respectively);
Subsequent hospital care services, with the limitation for the patient's admitting practitioner of one telehealth visit every 3 days (CPT codes 99231, 99232, and 99233); and
Subsequent nursing facility care services, with the limitation for the patient's admitting practitioner of one telehealth visit every 30 days (CPT codes 99307, 99308, 99309, and 99310).
Furthermore, CMS is revising §410.78(b) and §414.65(a)(1) accordingly. Specifically, the agency is adding individual and group KDE services, individual and group DSMT services, group MNT services, group HBAI services, and subsequent hospital care and nursing facility care services to the list of telehealth services for which payment will be made at the applicable PFS payment amount for the service of the practitioner. In addition, CMS reordered the listing of services in these two sections and removed "initial and follow-up inpatient telehealth consultations furnished to beneficiaries in hospitals and SNFs" in §410.78(b) because these are described by the more general term "professional consultations" that is in the same section. Finally, CMS is continuing to specify that the physician visits required under §483.40(c) may not be furnished as telehealth services.
The telehealth originating site facility fee was raised to $24.10.
The full final rulemaking is available at http://www.ofr.gov/OFRUpload/OFRData/2010-27969_PI.pdf with the major telehealth section from pages 486 to 526. There are other provisions addressing more specific forms of telehealth, such as cardiac event monitoring.
This final rule is scheduled to be printed in Federal Register on November 29, 2010.
CMS has proposed the following (8) additions to the list of approved procedures delivered via telehealth for 2011.
- Individual kidney disease education (KDE) services;
- Individual diabetes self-management training (DSMT) services;
- Group KDE, DSMT, MNT, and HBAI services;
- Initial, subsequent, and discharge day management hospital care services;
- Initial, subsequent, and other nursing facility care services;
- Neuropsychological testing services;
- Speech-language pathology services; and
- Home wound care services.
CMS is proposing to add the following requested services to the list of Medicare telehealth services for CY 2011:
- Individual and group KDE services (HCPCS codes G0420 and G0421, respectively);
- Individual and group DSMT services, with a minimum of 1 hour of in-person instruction to be furnished in the year following the initial DSMT service to ensure effective injection training (HCPCS codes G0108 and G0109, respectively);
- Group MNT and HBAI services (CPT codes 97804, and 96153 and 96154, respectively);
- Subsequent hospital care services, with the limitation for the patient’s admitting practitioner of one telehealth visit every 3 days (CPT codes 99231, 99232, and 99233); and
- Subsequent nursing facility care services, with the limitation for the patient’s admitting practitioner of one telehealth visit every 30 days (CPT codes 99307, 99308, 99309, and 99310).
Specifically, CMS is proposing to add individual and group KDE services, individual and group DSMT services, group MNT services, group HBAI services, and subsequent hospital care and nursing facility care services to the list of telehealth services for which payment will be made at the applicable PFS payment amount for the service of the practitioner. In addition, we have reordered the listing of services in these two sections and removed ‘‘initial and follow-up inpatient telehealth consultations furnished to beneficiaries in hospitals and SNFs’’ in § 410.78(b) because these are described by the more general term ‘‘professional consultations’’ that is in the same section. Finally, CMS is continuing to specify that the physician visits required under § 483.40(c) may not be furnished as telehealth services.
Here is a good article by Troy Heidesch which explains why Skype security is not up to tele-mental health standards.
Here are the differences between Secure Telehealth and Skype:
- Secure Telehealth quality is better (larger, clearer full-screen video image with less latency + better audio)
- Secure Telehealth security is significantly better (better encryption, no bouncing our signal off unknown supernodes).
- Secure Telehealth allows more than two participants. We routinely use this feature to provide training and support. The best training and support are provided when we can meet collectively in a video conference with both endpoints present with us. Note: many Secure Telehealth clients use our multi-party call feature for clinical and/or administrative meetings, such as for ACT team meetings.
- Secure Telehealth has option to move our service into your private network if/when you grow into this option. Skype cannot do this.
- Functionality - with Secure Telehealth, you can securely share powerpoints, your desktop, documents, videos, etc. with all participants. Skype cannot do this.
Secure Telehealth includes unlimited user support and training for all endpoints in our price (inside and outside your organization). If physicians outside of your organization have problems or questions, they may contact us directly for prompt resolution. With Skype you are on your own.

We'll be in Orlando on November 18-21, presenting at the US Psychiatric and Mental Health Congress.
Will you be there?
For more information, click here: http://www.cmellc.com/psychcongress/index.html

